The anatomy of the elbow joint.
The elbow joint is what is called a hinge joint, in that it only allows movement in one plane of motion. There are 3 bones involved which are the humerus, ulna and radial bones. The radius and ulna articulate with each other in two areas of the forearm at both ends this allows for the movement of supination and pronation (which basically is turning your hand facing up or down) both bones articulate with the end of the humerus bone.
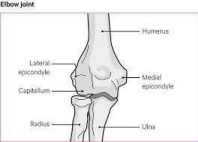
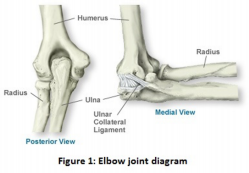
There are two bony prominences at the end of the humeral bone. There is one on the outer side which is the lateral epicondyle and one on the inner side which is the medial epicondyle. These structures are extremely important as they are the primary 2 areas that allow the attachment of tendons that act to move the forearm muscles.
In particular the lateral epicondyle muscles act to extend the forearm muscles and the medial epicondyle act to flex the forearm muscles.
What is Tennis Elbow?
Lateral epicondylitis is the term used to describe the presence of pain and a loss of function to the tendons of the outer elbow of the extensor muscle group of the forearm.
Tennis elbow is a repetitive overuse injury that can last anywhere from weeks to months or years and occurs predominantly between the ages of 30 to 50 years old, although can affect anybody at any age. There is an increased risk of developing tennis elbow in jobs, sports and occupations that utilize excessive wrist or hand usage.
Tennis elbow is to be considered a tendinopathy rather than true inflammation because the condition itself affects the tendons of the arm and is not underpinned by a true inflammatory process. Within the last few years research suggests that the condition shares similarities with hyperalgesia (hyper sensitive) pain conditions as a person’s sensory processing has shown to be altered compared to those without tennis elbow.
Symptoms of tennis elbow
- Localised tenderness and soreness on the outer side of the elbow
- Pain aggravated by wrist movements such ad grabbing, twisting and bending
- Clear history of overuse or overload with a gradual onset. LE can occur in both sedentary individuals with low levels of activity and also manual or labour intensive individuals but will require high levels of overload.
- Grip strength will not be affected although pain will be present when gripping, using maximal grip strength can irritate the tendon for days thereafter
How is tennis elbow diagnosed?
Tennis elbow is diagnosed when there is a clear history of overuse of the forearm muscles and wrist movements that is seen in correlation with a person’s occupation, lifestyle and general daily activities of daily living. Pain must be present on the outer side of the elbow and be aggravated by wrist movement and activity.
Imaging is not an accurate way to diagnose LE as degeneration has been shown to be present in both those with and without those with lateral elbow pain. However, imaging may be helpful to investigate further if conservative treatment has not shown improvements for some time.
Causes of Tennis elbow
Tennis elbow is a condition that develops over time which is often work related. It occurs due to overuse of the forearm muscles and tendons. When it comes to tendons, not all tendons do the same thing or have the same structure. For example tendons in the knee and ankle have different functions to those in the upper limb and therefore should be treated with the specific structure and function in mind.
When it comes to elbow extensors, the function is to hold the wrist still and stable with what we call an isometric contraction (contraction without movement) whilst gripping and hand movements.With tennis elbow, the common extensor tendon and in particular the ECRB (extensor carpi radialis brevis) is the main muscles of the elbow affected.
There is no concrete reason as to why LE develops in some individuals more than others. Wear and tear of tendons is a normal process with aging and tendons also adapt to the type of load they receive and this is evident in sports and various occupations. In regards to LE, some degeneration may be present although it has been suggested that not all people are predisposed to get pain.
Just like any other tendinopathies there are stages of progression. There is always a reactive phase, a tendon disrepair phase and degenerative phase. In the reactive phase rest and reduced activity has been shown to be very effective. However with the degenerative phase,
wear and tear on the tendon has already occurred. Treatment should aim to improve function and decrease pain with the appropriate management and loading strategies.
There are proposed mechanisms as to why tendinopathy develops although there is no concrete evidence of the exact pathway. A lot of Ebanie Rio and Jill Cook’s work suggest that it is a cell- initiated process when cells and tissues start to adapt to the specific stresses or load placed upon them.
There is an increased specific cell types of the surrounding area which leads to increased growth of blood vessels and nerves. This production also has the effect of collagen matrix. Pain and overload is the driving factor for this process to continue and worsen.
Is tennis elbow a lost cause?
There is a saying that goes ‘treat the donut and not the hole’ now adopted by many tendon experts such as Jill Cook and Ebonie Rio. What this means is that although there may be degeneration of some tendon tissue this does not predispose someone to disability and loss of function as there are healthy area’s of the tendon that have still have great capacity to become strong and functional without pain. Essentially, even though the tendon may show signs of tissue changes on an image it does not mean it necessarily will forever be painful.
Tennis elbow is commonly associated with these sports and activities:
- Tennis
- Racquetball
- Squash
- Fencing
- Weight lifting
And also activities or hobbies like:
- Carpentry
- Typing
- Painting
- Drilling
- Knitting
What are the best treatments for tennis elbow?
Exercise for tennis elbow
Exercise has been shown to be very effective for the treatment of lateral epicondylitis.This simply involves selecting the most appropriate exercise selection and proper progression with the aim of challenging the tissues to get stronger by creating adaptations to the exercises.
As compared to other treatment types exercise has been shown to be the most effective than any other treatment type.
For lateral epicondylitis the progression of exercise would look like wrist isometrics, wrist curls, resisted twisting (aka pronation and supination) and then grip training.
Massage and manual therapy for tennis elbow
Manual therapy has been shown to be a very effective treatment method for lateral epicondylitis. Chiropractors and physiotherapists adopt and utilise a range of manual therapy and exercise techniques like dry needling, joint mobilisation, assisted stretching, myofascial release therapy and even exercise therapy.
Research suggests that tendinopathy is a loading issue and it should be noted that loading or exercise will ultimately be what the tendon needs to bounce back from pain.
Sports chiropractors in particular have a much wider understanding of movement and corrective exercise when it comes to athletes and therefore are more equipped to treat those with sport related injuries.
Corticosteroid injection for tennis elbow
Corticosteroids have been found helpful to reduce pain and improve function short term (2-6weeks). They may provide temporary relief from pain for a few weeks although investigations of the long term effects of corticosteroids suggest that it may actually be the same in long term periods.
It has been shown that after a 12 week period after taking corticosteroid injections for tennis elbow, many people were the same and others worse than before the treatment was administered in clinical trials.
This suggests exercise therapy may be superior for long term outcomes as compared to corticosteroid injections.
Pulsed Ultrasound therapy for tennis elbow
Pulse ultrasound therapy like laser therapy have actually been shown to improve short term outcomes of patients with long standing LE. Although it should be noted that long term outcomes pulsed ultrasound therapy has limited evidence for improved outcomes.
Kinesio Taping for tennis elbow
Kinesio taping is a great tool to use when appropriate. In order to offload certain areas of excessive stress or using it may be helpful to reduce pain in these areas. Although much like manual therapy and passive treatment types, a proper loading progression is ultimately what will lead to better long term outcomes as the tissues have become stronger and more capable to tolerate more stress and load.
Orthoses or braces for tennis elbow
Orthoses and bracing has been shown to have some benefit in those with LE in the short term but little in long term. This may come down to offloading the structures by entirely incapacitating the joints and tissues.
Acupuncture for tennis elbow
There is mild evidence to suggest that acupuncture may help decrease pain from a few days, weeks and rarely months. This is probably one of the last researched treatment methods here. As another form of manual therapy, long term outcomes have not been thoroughly investigated.
Surgery for tennis elbow
When conservative treatment has exceeded 12 months with little to no improvements in pain and function, surgery has actually been shown to have some benefit. It should be noted that surgery is the last resort when all else fails. There is very few studies that have investigated the effects of surgery for LE 6 to 12 months later.
Other considerations
Tennis elbow is a condition which can last from weeks to months and even years. Failed attempts at conservative care for at least 6 months may but not always omit the use of surgery as a means to treat the condition. It has been found that in long standing causes the removal diseased muscle and also reattaching healthy muscle to the tendon again.
Although this a very unlikely occurrence it should be noted that this is not always necessary and that conservative care using non-invasive methods should always be the primary option.
Referenes
1. Johnson GW, Cadwallader K, Scheffel SB, Epperly TD. Treatment of lateral epicondylitis. Am Fam Physician. 2007;76(6):843-8.
2. Juul-Kristensen B, Lund H, Hansen K, Christensen H, Danneskiold-Samsøe B, Bliddal H. Poorer elbow proprioception in patients with lateral epicondylitis than in healthy controls: a cross-sectional study. J Shoulder Elbow Surg. 2008;17(1 Suppl):72S-81S.
3. Ahmad Z, Siddiqui N, Malik SS, Abdus-Samee M, Tytherleigh-Strong G, Rushton N. Lateral epicondylitis: a review of pathology and management. Bone Joint J. 2013;95-B(9):1158-64.
4. Cullinane FL, Boocock MG, Trevelyan FC. Is eccentric exercise an effective treatment for lateral epicondylitis? A systematic review. Clin Rehabil. 2014;28(1):3-19.
5. Knutsen EJ, Calfee RP, Chen RE, Goldfarb CA, Park KW, Osei DA. Factors associated with failure of nonoperative treatment in lateral epicondylitis. Am J Sports Med. 2015;43(9):2133-7.
6. Pitzer ME, Seidenberg PH, Bader DA. Elbow tendinopathy. Med Clin North Am. 2014;98(4):833-49, xiii.
7. Eraslan L, Yuce D, Erbilici A, Baltaci G. Does Kinesiotaping improve pain and functionality in patients with newly diagnosed lateral epicondylitis? Knee Surgery, Sports Traumatology, Arthroscopy. 2018;26(3):938-45.
8. Lai WC, Erickson BJ, Mlynarek RA, Wang D. Chronic lateral epicondylitis: challenges and solutions. Open Access J Sports Med. 2018;9:243-51.
9. Bisset LM, Vicenzino B. Physiotherapy management of lateral epicondylalgia. J Physiother. 2015;61(4):174-81.
10. Fernández-Carnero J, Fernández-de-las-Peñas C, Sterling M, Souvlis T, Arendt-Nielsen L, Vicenzino B. Exploration of the extent of somato-sensory impairment in patients with unilateral lateral epicondylalgia. J Pain. 2009;10(11):1179-85.
11. Lim ECW, Sterling M, Vicenzino B. Chronic Lateral Epicondylalgia Does Not Exhibit Mechanical Pain Modulation in Response to Noxious Conditioning Heat Stimulus. Clin J Pain. 2017;33(10):932-8.
